The recent outbreak of the Marburg virus in Rwanda, claiming eleven lives and confirming thirty-six cases, underscores the urgent need to understand this deadly hemorrhagic fever. While rare, its highly contagious nature and potential for widespread devastation demand immediate attention. The lack of a readily available vaccine or treatment further complicates the situation, highlighting the vulnerability of populations facing such outbreaks, particularly in resource-constrained settings. Understanding the transmission, symptoms, and potential preventative measures is crucial in curbing the spread and minimizing its impact. This analysis explores the key aspects of the Marburg virus, examining its transmission, symptoms, and the current challenges in managing outbreaks.
Understanding Marburg Virus Transmission
Zoonotic Origin and Human-to-Human Transmission
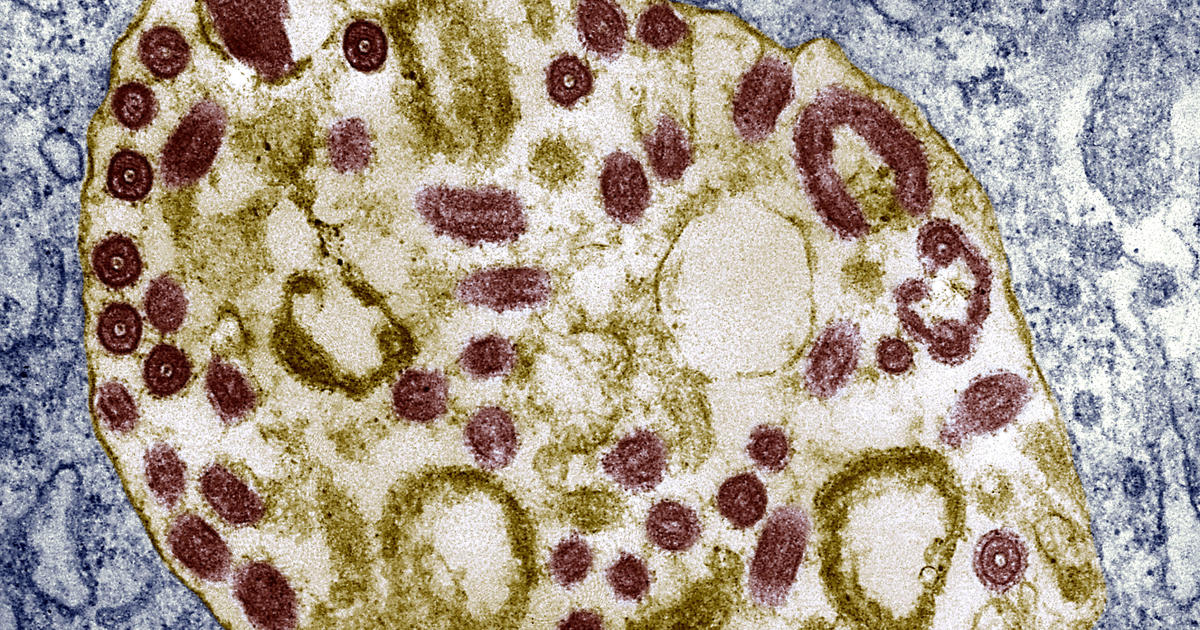
The Marburg virus, like its cousin Ebola, is a zoonotic disease, meaning it originates in animals and then transmits to humans. Fruit bats are identified as the natural reservoir. However, human-to-human transmission is the primary driver of outbreaks. This transmission occurs primarily through direct contact with the bodily fluids of an infected person (blood, vomit, feces, urine, sweat, saliva, breast milk), or contaminated surfaces and materials like bedding, clothing, medical equipment, and even needles. The virus does not spread through the air, unlike some other respiratory viruses, which reduces the likelihood of airborne spread. However, close proximity and direct contact are sufficient for infection. This underscores the importance of strict infection control measures in healthcare settings and communities with suspected cases. Effective contact tracing and quarantine measures are therefore crucial in controlling the spread among human populations.
The Importance of Infection Control and Prevention Measures
Containing the spread of Marburg virus heavily relies on stringent infection control and preventative measures. These include the immediate isolation of infected individuals, safe burial practices for victims, and thorough disinfection of contaminated areas. Healthcare workers treating infected patients must use personal protective equipment (PPE), such as gloves, gowns, masks, and eye protection, to minimize their risk of exposure. Furthermore, the education of the public about the risks and preventative measures, such as handwashing, avoiding contact with potentially infected animals and practicing safe hygiene, plays a crucial role in reducing the possibility of further transmission. Robust surveillance and rapid response are critical in early detection and containment of outbreaks, especially in regions with limited healthcare infrastructure. Early detection also helps in limiting widespread community spread and potential mortality.
Recognizing Marburg Virus Symptoms and Stages
Early Symptoms: Mimicking Other Illnesses
Initially, symptoms of Marburg virus disease (MVD) might resemble those of other illnesses like malaria or influenza. These early symptoms typically emerge within 3 to 21 days after exposure and include fever, severe headache, muscle aches, and malaise. These non-specific symptoms can easily be mistaken for common viral illnesses, delaying diagnosis and the timely implementation of containment measures. This makes prompt detection a critical component in managing and containing potential outbreaks. Any individual exhibiting these symptoms in a region with potential exposure risk should seek immediate medical attention to ensure appropriate testing and early intervention.
Late Stage Manifestations: Severe Illness and Hemorrhagic Complications
As the disease progresses, the symptoms become more severe and more distinctly indicative of Marburg virus infection. These may include nausea, vomiting, chest pain, abdominal pain, severe diarrhea, and skin rashes. The distinctive, severe and often fatal late-stage manifestations involve internal and external bleeding (such as bleeding from the gums, nose, and anus), which stems from impaired clotting factors. Severe cases also frequently exhibit jaundice (yellowing of the eyes and skin), delirium and organ failure, ultimately resulting in shock and death. The severity of the later stages highlights the need for rapid detection, isolation, and supportive care to manage potential complications and to reduce mortality rates.
Challenges in Managing Marburg Virus Outbreaks
Absence of Approved Treatments and Vaccines
One significant hurdle in tackling Marburg virus outbreaks is the lack of any authorized vaccines or specific treatments. Current efforts focus on supportive care, providing intravenous fluids to manage dehydration, maintaining blood pressure and electrolyte balance, and mitigating organ failure complications. These therapies merely support the patient through the disease but do not directly tackle the virus itself. The absence of proven and effective antiviral therapies represents a pressing challenge in addressing the disease’s fatality rate, which has historically been quite high. Investing in research and development for vaccines and effective treatment options are essential.
Limitations in Healthcare Infrastructure
The impact of a Marburg virus outbreak is greatly exacerbated by inadequate healthcare infrastructure, especially in resource-constrained settings. Lack of access to timely and accurate testing, limited intensive care capacity, and a shortage of trained healthcare personnel pose significant obstacles to managing the disease effectively. The potential for rapid disease progression underscores the need to prepare medical facilities and staff to handle both suspected and confirmed cases, to minimize mortality and spread. Providing well-trained personnel, reliable testing mechanisms, appropriate isolation equipment and essential medical supplies in preparation for a potential outbreak is a vital preemptive strategy.
Take Away Points
- Marburg virus is a highly contagious hemorrhagic fever with a high mortality rate.
- Transmission occurs through direct contact with bodily fluids of infected individuals or contaminated surfaces. It is not airborne.
- Early symptoms are nonspecific and can be mistaken for other illnesses. Later-stage symptoms include severe hemorrhagic complications and organ failure.
- Currently, there are no licensed vaccines or treatments for Marburg virus; supportive care is the mainstay of management.
- Effective outbreak response relies on rapid diagnosis, strict infection control, contact tracing, and strengthened healthcare infrastructure.